Section 2
Guidelines for Prevention and Control of Communicable Diseases
A. Prevention and Control of Communicable Diseases in Schools and Child Care Facilities
B. Covering Your Cough
- Why should I cover my cough?
- Serious respiratory illnesses like Influenza, Respiratory Syncytial Virus (RSV), Tuberculosis and Severe Acute Respiratory Syndrome (SARS) are spread by coughing or sneezing.
- These illnesses can be spread to others when the ill person coughs or sneezes germs into the air where other people breathe them in or cough or sneeze into their hands and then contaminates surfaces and objects that are touched by others.
- These illnesses spread easily in crowded places where people are in close contact.
- How do I stop the spread of germs if I am sick?
- Cover your nose and mouth with a tissue every time you cough or sneeze. Throw the used tissue in a waste basket.
- Sneeze or cough into your upper sleeve or the crook of your arm if you do not have a tissue, not your hands.
- Clean your hands with soap and water (or an alcohol-based hand rub if soap and water are not available) immediately after coughing or sneezing.
- Stay home when you are sick; keep your distance from others to protect them from getting sick too.
- Do not share eating utensils, drinking glasses, towels or other personal items.
- Clean and disinfect surfaces and objects that could be contaminated by an ill person.
- How can I stay healthy?
- Clean your hands often with soap and water; if soap and water are not available, use an alcohol-based hand sanitizer.
- Avoid touching your eyes, nose, or mouth.
- Avoid close contact with people who are sick, if possible.
- Get vaccinated! Influenza (flu), pneumococcal (pneumonia), and pertussis (whooping cough) vaccines can prevent some serious respiratory illnesses.
- When you are at the clinic or hospital:
- Cover your cough or sneeze into a tissue and dispose of the used tissue in the waste basket.
- Clean your hands with soap and water; if soap and water are not available, use an alcohol-based hand rub.
- You may be asked to wear a mask to protect others.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
C. Cover Your Cough Poster

D. Gloving
The following information is provided as general recommendations. Always follow the glove use policies established by your facility.
- General information
- Gloves are NOT a substitute for hand washing.
- Throw away single-use gloves after each use and if torn.
Removing single-use gloves:
1) Grasp outside edge near wrist.
2) Peel away from hand turning glove inside-out.
3) Hold in opposite gloved hand.
4) Slide ungloved finger under the wrist of the remaining glove, be careful not to touch outside of glove.
5) Peel off from inside, creating a bag for both gloves.
6) Discard glove and wash hands thoroughly.
- Hands must be washed with soap after removing gloves.
- Use non-latex gloves when touching people or food whenever possible.
- Gloves should fit properly and comfortably.
- Gloves should be durable, so they do not rip or tear during use.
- Types and use of gloves
- Medical glove (e.g., surgical glove, examination glove)
- Used for exposure-related tasks where there is contact with blood and body fluids. For example, when handling blood (e.g., nosebleeds, cuts) or items, surfaces, or clothing soiled by blood or bloody body fluids, follow procedures outlined in the childcare or school’s Bloodborne Pathogen Exposure Plan.
- Used when changing the diaper of a child with diarrhea or with an infection that is spread through stool, or if the child has open areas on the skin.
- Worn by staff if they have open cuts, sores, or cracked skin.
- Plastic film food handling gloves are not considered appropriate for use for the above-mentioned activities.
- Utility gloves
- Used for cleaning and disinfecting bathrooms, diapering areas, and any areas contaminated with stool, vomit, or urine.
- After use, follow cleaning and disinfecting procedures.
- Food handling gloves
- Recommended or required for handling ready-to-eat foods in some jurisdictions.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
E. Hand Washing
- General information
Hands are parts of the body that come into frequent contact with germs that cause communicable illnesses. Young children might not have learned and be aware of healthy personal habits.
Young children suck their fingers and/or thumbs, put things in their mouths, and rub their eyes. These habits can spread disease, but frequent and good hand washing can help reduce infection due to these habits. Caregivers who teach and model good hand washing techniques can reduce illness in childcare settings and schools.
Gloves are not a substitute for hand washing. Hand washing is the single most effective way to prevent the spread of infections. Included in this section are instructions on WHEN to wash hands and a picture to demonstrate HOW TO do the correct hand washing procedure (see section II-C).
- Childcare and school staff information
- Learn why, how, and when to correctly wash their hands and the children’s hands.
- Follow a procedure that ensures safety for the infant or child.
- Teach young children to wash their hands and supervise them as they do.
- Encourage children to wash hands frequently.
- Recommendations for hand hygiene products
- Liquid soap
– Recommended in childcare and schools since used bar soap can harbor bacteria. Regular liquid soap is effective in removing soil and germs.
-
- Soap and water are necessary when hands are visibly soiled.
- When using liquid soap dispensers, avoid touching the tip of the squirt spout with hands.
- If the liquid soap container is refillable, the container and pump should be emptied, cleaned, and dried completely before being refilled.
- Antimicrobial soaps
- Not recommended by the American Medical Association and the CDC.
- Many scientists are concerned that use of these soaps could lead to strains of resistant bacteria. There is no need to use these soaps, which may do more harm than good.
- Must be left on hands for about two minutes to have any effect on bacteria.
- Alcohol-based hand rubs (Sanitizers)
- Use 60% to 90% alcohol (usually 70%). Read the label and follow manufacturer’s instructions.
Advantages of alcohol-based hand rubs are:
- Require less time and are more accessible than sinks for hand washing with soap and water.
- Reduce bacterial counts on hands.
Disadvantages of alcohol-based hand rubs are:
- Should not be used on visibly soiled hands since they are ineffective in the presence of dirt, soil, or food.
- Can reduce the number of germs on hands in some situations, but sanitizers do not eliminate all types of germs.
- Alcohol-based hand rubs should be safely stored out of reach of children.
Procedure for using alcohol-based hand rubs:
- Apply enough alcohol-based hand rub to palm of one hand to wet both hands completely.
- Rub hands together covering all surfaces of hands and fingers.
- Continue rubbing over all surfaces of both hands and fingers until hands are dry.
- When soap and running water are not available
- For example, on a field trip, an alcohol-based hand rub can be used. The alcohol-based hand rub must be applied vigorously over all hand surfaces.
- If hands are visibly soiled, hands must be washed with soap and warm running water as soon as it is available, because the alcohol-based hand rubs are ineffective in the presence of dirt and soil.
- Hand sanitizers should not be used as a replacement for thorough hand washing under warm running water when available. No chemical substitute (sanitizer solutions) is as effective as running water.
- DO NOT use a common water basin. The water can become contaminated very quickly.
- Towels
- Use single-use paper towels to dry hands or use hand dryers.
- DO NOT use multi-use towels such as hand towels, kitchen towels, or dish cloths.
- Fingernail care for staff and children
- Keep fingernails short and clean.
- Staff should moisten cuticles with a moisturizer to avoid hangnails.
- Clear fingernail polish that is well maintained may be worn; avoid colored nail polish since it is difficult to see dirt under nails.
- Use fingernail brushes to remove dirt and stool from under nails. Use the nailbrush after diapering or assisting with the toilet activities, before and after food preparation, and whenever nails are soiled.
- Artificial nails are highly discouraged as they are known to harbor germs even with good hand washing techniques. They can break off into food and have been implicated in disease outbreaks in hospitals.
- Check with the local licensing agency regarding any food codes that may restrict staff from wearing artificial nails when handling and preparing food.
- Caregiver training on how to wash hand.
- How to wash the hands of children at a sink?
Caregivers should train children who are developmentally able to learn personal hygiene. This training program should teach the following hand washing procedures.
- Wet hands with warm running water and apply soap.
- Rub hands together with soap vigorously for 20 seconds.
- Rinse hands well under warm running water.
- Dry hands using a single-use paper towel or air dryer.
- How to wash the hands of infants?
Caregivers should wash the hands of infants, who are unable to wash their own hands and who are too heavy to hold safely at the hand washing sink, as follows:
- Thoroughly wipe the child’s hands with a disposable wipe; or
- Thoroughly wipe the child’s hands with a damp single-use towel, moistened with liquid soap. Then wipe the child’s hands with a damp single-use towel until the child’s hand is free of soap. Then use a dry paper towel to dry the child’s hands.
- When to wash hands.
Caregivers should wash their hands under any of the following conditions:
- Any time their hands come into contact with blood, mucus, vomit, feces or urine.
- Before preparing or handling food.
- Before engaging in any activity related to serving food, including, without limitation, setting the table.
- Before and after eating a meal or snack.
- After using the toilet, helping a child use the toilet, changing a diaper with or without gloves, or assisting a child with hand washing.
- After attending to an ill child.
- After handling an animal.
- After handling garbage.
- After cleaning contaminated or soiled surfaces.
- Before and after giving medication.
- Anytime hands become visibly soiled.
Children should wash their hands under any of the following conditions:
- Any time that their hands come into contact with blood, mucus, vomit, feces, or urine or garbage.
- Before handling food.
- Before and after eating a meal or snack.
- After outdoor play.
- After handling an animal.
- After the diaper or underwear is changed and/or after using the toilet.
- After playing in water.
- After playing in a sandbox.
- Anytime hands become visibly soiled.
- Ways for staff to keep hands healthy
- Cover open cuts and abrasions less than 24 hours old with a dressing (e.g., bandage).
- Use warm water, not extremely hot or cold and just enough soap to get a good lather.
- Rinse and dry hands completely.
- Use the soap product that is least drying to hands.
- Use hand lotion regularly to keep skin moist. Use products with a squirt spout so the hands do not have contact with the container.
- Wear gloves outside in the cold weather.
- Wear utility gloves for direct hand contact with harsh cleaners or chemicals.
- Wear work gloves when doing yard work, gardening, etc.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
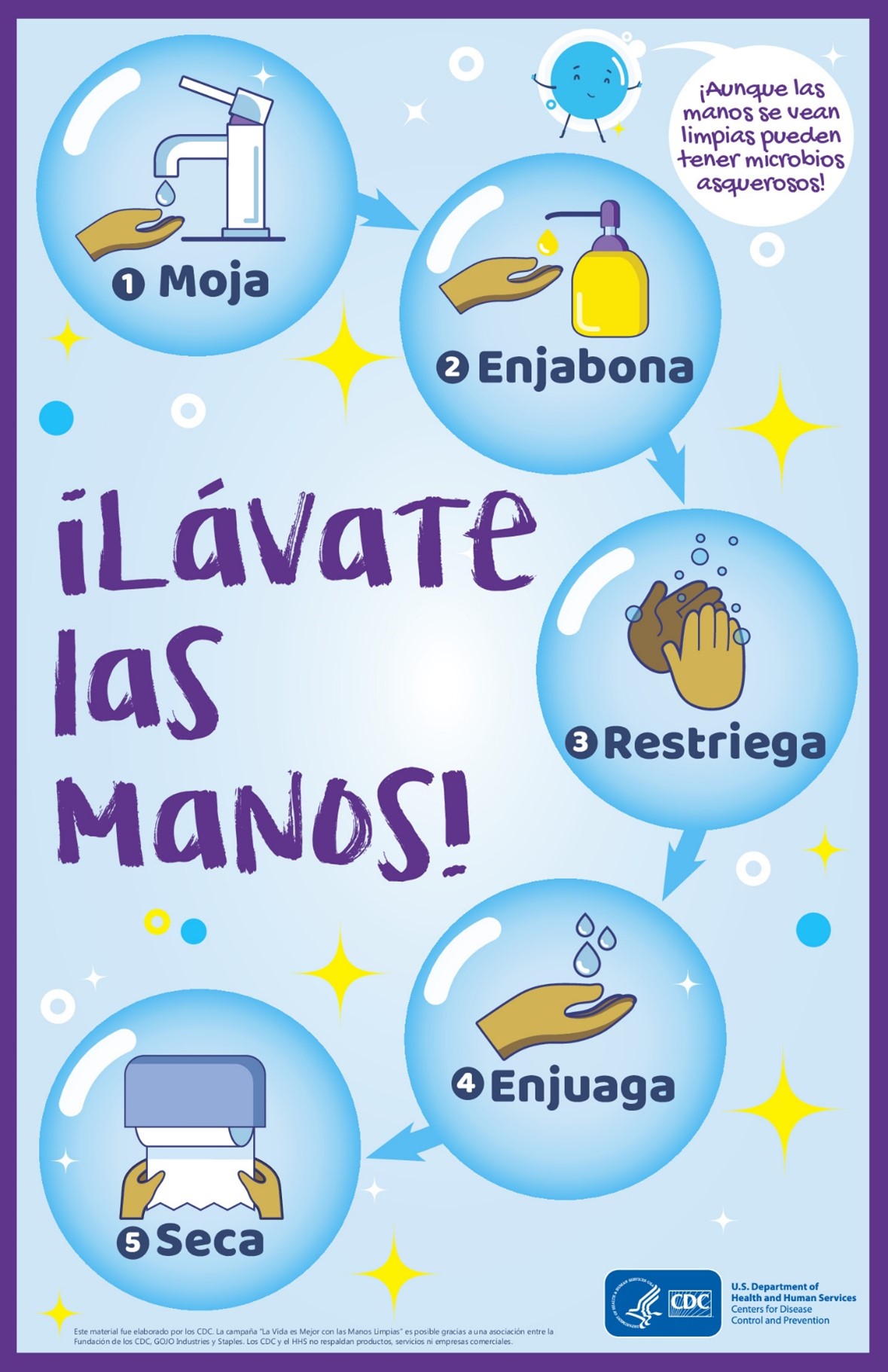
F. Handwashing Poster
English

Spanish
HANDWASHING
The single most effective thing that can be done to prevent the spread of disease is to correctly wash your hands thoroughly and often.
Both STAFF and CHILDREN WASH:
- When arriving.
- Before and after eating, before preparing or serving food, or setting the table.
- Before and after preparing or giving medication.
- After using the toilet, before and after diaper change, or after assisting a child with toilet use.
- After handling items soiled with body fluids or wastes (blood, vomit, stool, urine, drool, or eye drainage).
- After coughing, sneezing, or blowing your nose.
- After playing with or caring for pets or other animals.
- After playing outside.
- Before and after using water tables or moist items such as clay.
- Whenever hands look, feel, or smell unclean.
- Before going home
G. Infection Control Guidelines
Sections I – III of this manual contains information on ways to reduce the spread of germs in childcare settings and schools.
Key concepts of prevention and control:
- Handwashing – the single most effective way to prevent the spread of germs.
- Covering your cough – an effective way to reduce the spread of germs when coughing and sneezing.
- Appropriate gloving – an effective way to help prevent the spread of germs. It is not a substitute for handwashing. See standard precautions below.
- Proper diapering procedures – to reduce the spread of germs from stool to hands, objects, and the environment.
- Cleaning, sanitizing, and disinfection – to reduce the presence of germs in the environment.
- Food safety – to reduce the spread of germs from improperly cooked, stored, and handled foods.
- Exclusion guidelines – to reduce the chance of spreading germs from ill people to others.
- Immunizations – for list of resources for age-appropriate immunizations and childcare and school requirements.
- Avoid sharing personal items – encourage children, students, and staff to NOT share items such as water bottles, food, utensils, beverages, straws, toothbrushes, lip gloss, lip balm, lipstick, towels, headgear, combs, brushes, etc. to prevent the spread of germs to others.
- Promote self-care – encourage staff and children to perform their own first aid when age appropriate.
- Standard Precautions are used in many settings where there is a possibility of exposure to blood and body fluids (e.g., urine, stool, secretions from the nose and mouth, drainage from sores or eyes). One aspect of standard precautions is the use of barriers. The purpose of using barriers is to reduce the spread of germs to staff and children from known/unknown sources of infections and prevent a person with open cuts, sores, or cracked skin (non-intact skin) and their eyes, nose, or mouth (mucous membranes) from having contact with another person’s blood or body fluids.
Examples of barriers that would be used for childcare and school settings include:
– Gloves (preferably non-latex) when hands are likely to be soiled with blood or body fluids.
– CPR (cardiopulmonary resuscitation) barriers
– CPR mask or shield.
Other examples that most likely would not be needed in the childcare or school setting are:
– Eye protection and a face mask when the face is likely to be splattered with another’s blood or body fluid.
– Gowns when clothing is likely to be splattered with another’s blood or body fluid.
Proper use of safety needle/sharp devices and proper disposal of used needles and sharps are also part of standard precautions.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
H. Infection Control Recommendations for School Athletic Programs
- General information
Students participating in school athletic programs may have increased risk of infection because of skin-to-skin contact or through the sharing of water bottles, athletic equipment, and towels. To minimize the risk of infection:
- Emphasize frequent hand washing and/or use of an alcohol-based hand sanitizer; if hands are visibly soiled, they must be washed using soap and water.
- Exclude athletes with non-intact skin (e.g., boils, sores, cuts, etc.) from competition or practice until evaluated by a healthcare provider.
- Exclude athletes with head lice from activities where there is head-to-head contact, or headgear is used until they are treated.
- Ensure that all athletes have their own water bottles and discourage the sharing of water bottles.
- Provide clean towels for athletes during practice and competition to minimize contact with the saliva and secretions of others.
- Encourage all persons to wear shower shoes, sandals, or flip-flops in the shower or the locker room to prevent the spread of fungal infections (athlete’s foot) and plantar warts.
- Inform athletes that items such as toothbrushes, razors, and nail clippers might be contaminated with blood and should not be shared.
- Cover breaks in skin with a water-proof bandage. Change bandage if it gets wet.
- Athletes with open wounds, whether covered or not, should not use athletic facility ice tubs or whirlpools.
- Disinfect frequently touched areas on shared equipment and in the athletic area daily using a commercial Environmental Protection Agency (EPA) – registered detergent disinfectant effective on Staphylococcus aureus, or a fresh (mixed daily) solution of one part bleach and 100 parts water (1 tablespoon bleach in one quart of water), on a clean surface, with a 10-minute wet contact time.
- Articles that come in contact with the wound should be washed, in the hottest water the fabric will tolerate, and then dried, using the hottest setting the fabric will tolerate.
- Have athletes shower after every practice/game. DO NOT share towels.
- Possible blood exposure
Participation in sports may result in injuries in which bleeding occurs. The following recommendations have been made for sports in which direct body contact occurs or in which an athlete’s blood or other body fluids may contaminate the skin or mucous membranes of other participants or staff:
- Have athletes cover existing cuts, abrasions, wounds, or other areas of broken skin with an occlusive dressing (one that covers the wound and contains drainage) before and during practice and/or competition. Caregivers should cover their own non-intact skin to prevent spread of infection to or from an injured athlete.
- Wear disposable gloves to avoid contact with blood or other body fluids and any object such as equipment, bandages, or uniforms contaminated with these fluids. Hands should be thoroughly cleaned with soap and water or an alcohol-based hand rub as soon as possible after gloves are removed.
- Remove athletes with active bleeding from competition as soon as possible and until the bleeding has stopped. Wounds should be cleaned with soap and water. Skin antiseptics may be used if soap and water are not available. Wounds must be covered with an occlusive dressing that remains intact during further play before athletes return to competition.
- Advise athletes to report injuries and wounds as soon as possible, including those that occur before or during competition.
- Clean and cover minor cuts or abrasions that are not bleeding or draining during scheduled breaks; this does not require interruption of play. However, if an athlete’s equipment or uniform fabric is wet with blood, the uniform should be removed and replaced, and the equipment should be cleaned and disinfected or replaced.
- Clean equipment and playing areas contaminated with blood until all visible blood is gone. Then disinfect with an EPA-approved disinfectant* (viricidal, bactericidal, fungicidal) OR make a bleach solution (3 tablespoons 8.25% household bleach to 1 gallon of water). If using the bleach solution, apply to the surface or area. DO NOT rinse. Air dry. The disinfected area should be in contact with the bleach solution for at least 1 minute. * EPA-approved disinfectants must be used according to the manufacturer’s recommendations.
- Have access to a well-equipped first aid kit during any adult-supervised athletic event. This includes personal protective equipment for first aid responders.
- DO NOT delay emergency care because gloves or other protective equipment are not available. If the caregiver does not have the appropriate protective equipment, a towel may be used to cover the wound until an off-the-field location is reached where gloves can be used during the medical examination and treatment.
- Follow current CPR guidelines.
- Train equipment handlers, laundry personnel, and janitorial staff in proper procedures for handling washable or disposable materials contaminated with blood. Staff should always wear gloves when handling items contaminated with blood.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
I. Misuse of Antibiotics
Antibiotic misuse has resulted in antibiotic-resistant bacteria that can cause severe infections and even result in death. Everyone (childcare staff, teachers, school nurses, parents/guardians, healthcare providers, and the community) has a role in preventing antibiotic misuse.
- Antibiotics and What Do They Do
- What kinds of germs cause infections? Viruses and bacteria are two kinds of germs that can cause infections and make people sick.
- What are antibiotics? Antibiotics are powerful medicines that are mostly used to treat infections caused by bacteria. These are known as anti-bacterial drugs. These drugs cannot fight viruses; there is a special class of medicines called antivirals that specifically fight infections caused by viruses. There are many classes of antibiotics, each designed to be effective against specific types of bacteria. When an antibiotic is needed to fight a bacterial infection, the correct antibiotic is needed to kill the disease-producing bacteria.
- When are antibiotics needed? Anti-bacterial drugs are needed when your child has an infection caused by bacteria. These drugs cannot fight infections caused by viruses.
- How can I tell if an illness is caused by a virus or bacteria? The symptoms of viral infections are often the same as those caused by bacterial infections. Sometimes diagnostic tests are needed, but it is important that your doctor or healthcare provider decide if a virus or bacteria is causing the infection.
- If an infection is caused by a virus, and an antibiotic will not work, what can be done to relieve the symptoms? You need lots of extra rest, plenty of fluids (water and juice), and healthy foods. Some over-the-counter medications, like acetaminophen (follow package directions or your healthcare providers’ instructions for dosage) or saline nose drops may help while your body is fighting the virus. A cool mist vaporizer may help too. Viral infections (like chest colds, acute bronchitis, and some sore throats) resolve on their own but symptoms can last several days or as long as a couple of weeks.
- When Antibiotics Are Needed
- Are antibiotics needed to treat a runny nose with green or yellow drainage? No. An antibiotic will not help. A runny nose is a common symptom of a chest cold or acute bronchitis. A runny nose may begin with clear drainage then turn to yellow or green drainage. Color changes in nasal mucous are a good sign that your body is fighting the virus. If a runny nose is not getting better after 10 to 14 days or if other symptoms develop, call your healthcare provider.
- Are antibiotics needed for a sore throat? Not usually. Most sore throats are caused by a virus and antibiotics will not help. Only throat infections caused by Group A strep bacteria need an antibiotic. Your healthcare provider can do a lab test. If Group A strep bacteria is present, they can prescribe an antibiotic.
- Does acute bronchitis need antibiotics? No. Most cases of acute bronchitis (another name for a chest cold) are caused by viruses, and antibiotics will not help. Children with chronic lung disease are more susceptible to bacterial infections and sometimes they need antibiotics.
- Does a sinus infection need antibiotics? Sometimes. Antibiotics are needed for sinus infections caused by bacteria; antibiotics are not needed for sinus infections caused by viruses. Check with your healthcare provider if cold symptoms last longer than 10 to 14 days without getting better or pain develops in your sinus area.
- Do ear infections need an antibiotic? Sometimes. Ear infections can be caused by bacteria or viruses, so not all ear infections need antibiotics. Your healthcare provider will need to assess your symptoms and determine whether antibiotics are needed.
- Antibiotic Resistance
- What are antibiotic resistant bacteria? Antibiotic resistant bacteria are germs that are not killed by commonly used antibiotics. These bacteria are very difficult to cure, and sometimes very powerful antibiotics are needed to treat infections caused by these bacteria.
- Is antibiotic resistance a problem? Yes. An increase in antibiotic resistance among bacteria that commonly cause disease has been seen throughout the U.S. – including Nevada. Antibiotic resistance is a growing problem as an ever-increasing number of bacteria are resistant to more than one type of antibiotic, making infections caused by these bacteria harder to treat.
- How do bacteria become resistant to certain antibiotics? There are three different ways that bacteria become resistant to antibiotics:
1) Taking antibiotics can increase your chance of developing antibiotic-resistant bacteria. Antibiotics kill the disease-causing bacteria, but they also kill some good bacteria. Some bacteria that have been exposed to the antibiotic have developed ways to fight them and survive. These bacteria become stronger, can multiply, and begin to cause symptoms. These resistant bacteria not only can cause you to be ill, but you can spread these resistant bacteria to others, and they too may become ill.
2) Antibiotic resistant infections can be spread from people or objects that are contaminated with resistant bacteria. These bacteria can enter your body when you touch these objects and then touch your mouth or nose or eat food with contaminated hands. The best way to prevent spreading any germs is to wash your hands!
3) Antibiotic-resistant bacteria can also out-smart the antibiotics designed to kill them. This happens when the bacteria inside your body share, exchange, or copy genes that allow them to survive the antibiotic.
- Are antibacterial products (e.g., antibacterial soaps) better than ordinary products? At home and in childcare and school settings, antibacterial (or antimicrobial) products are no better than ordinary soap for preventing infections.
- Why should I be concerned about antibiotic resistance? Improper use of antibiotics can cause more frequent and possibly more severe illness for you and your family. Antibiotic misuse also is bad for your community by increasing the number of bacteria that are hard for healthcare providers to treat.
- What if I get sick with an antibiotic-resistant infection? Antibiotic-resistant bacterial infections require stronger antibiotics. These medications often must be given through a vein and may require a hospital stay. They may also cause more severe side effects. Antibiotic-resistant infections of the blood or brain can be life threatening.
- How Can I Prevent Antibiotic-Resistant Infections?
- Use antibiotics only when your healthcare provider prescribes them – and always take all the medicine that is prescribed.
- Never ask for antibiotics for a viral infection such as a cold, acute bronchitis, cough, or green/yellow runny nose.
- Never let anyone take leftover antibiotics or a prescription that was used by someone else in your household. – Hand washing helps prevent the spread of infections! Wash your hands thoroughly – and teach your children to wash their hands too – using soap and running water for 20 seconds after blowing your nose, after using the toilet and after changing diapers, and before preparing food or eating.
- Appropriate Use of Antibiotics
- Are antibiotics safe? Yes. Antibiotics taken as prescribed are generally safe and effective at combating bacterial infections. Some people may be allergic to certain antibiotics but can usually take other types of antibiotics if needed. All medications can have side effects, so be sure to ask your healthcare provider about potential side effects and how to manage them.
- When should I take antibiotics? You should take antibiotics – the complete prescription – when your healthcare provider prescribes them for a bacterial infection. Never save antibiotics for a later use.
- When I’m feeling better can I stop taking the antibiotic? No, not before you complete all the medication prescribed. The prescription is written to cover the time needed for your body to completely kill the bacteria. If you stop taking the antibiotic early, the bacteria that are still alive are more likely to be resistant and could restart the infection – or be passed on to others.
- Appropriate Storage of Antibiotics
- Can antibiotics be stored in other than their original containers? You should always store antibiotics in their original containers. If children are present antibiotics should be stored with child-resistant caps.
- Where should antibiotics be stored? Antibiotics should be stored in an organized fashion, away from food, at the proper temperature, and in an area inaccessible to children.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
J. Human Biting Incidents
Biting can be a common occurrence in the childcare and school setting. The risk of getting hepatitis B virus (HBV) or Human Immunodeficiency Virus (HIV) from a bite is extremely low for either the child who did the biting or the child or staff member who was bitten. It is very difficult to spread these viruses by biting.
In addition, most infants are now being vaccinated against the hepatitis B virus and the number of preschool children (3 to 5 years) with chronic hepatitis B infection is expected to be low. However, biting is more likely to cause an infection at the bite site.
Written policies and procedures should be in place before biting incidents occur to ensure proper communication with parents/guardians and staff.
Childcare and school staff, what to do if a biting incident occurs in the childcare or school setting:
- Determine if the bite broke the skin (produced an open wound or puncture wound) and/or caused bleeding.
- Wear gloves when providing immediate first aid to the bite wound. The wound should be carefully cleaned with soap and water.
- Inform parents/guardians of both children involved in the biting incident when two children are involved in the incident. This should be done as soon as possible.
- If the bite broke the skin, it is recommended that the family or staff consult with a healthcare provider as soon as possible for any further instructions.
- DO NOT share the names or any information about the children involved in the biting incident. Release of any information may be a breach of confidentiality or data privacy.
- Document the incident in writing as established by your facility’s policy.
Reasons parent/guardian or staff members should call healthcare provider:
- To determine if blood tests and/or treatment are needed. It is unlikely that the bite will be the source of infection for hepatitis B or HIV, but each situation must be looked at on a case-by case basis.
- If the bitten person is not up to date for tetanus/diphtheria/pertussis and hepatitis B vaccinations. The person should receive these vaccines as soon as possible.
- If the bitten person has any of the following signs of infection:
– Increased swelling, redness, warmth, or tenderness at the site.
– Pus at the site.
– Fever of 100°F or higher.
If any of these symptoms occur or if the bitten person begins to act sick or the wound does not heal, call the healthcare provider immediately.
Prevention and Control
- Parents/guardians and childcare and school staff should develop a behavior modification plan to prevent further incidents.
- A child who is infected with HIV or hepatitis B virus and continues to bite should be assessed by a team of medical experts to determine an appropriate response plan to prevent the risk of spread of these viruses.
Call your childcare health consultant or your local or state health department for additional assistance with these incidents.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov

