Monkeypox Virus Guidance: Infection Control and Prevention in Health Care Settings
Background
Standard Precautions should be applied for all patient care, including for patients with suspected monkeypox. If a patient seeking care is suspected to have monkeypox, infection prevention and control measures should be implemented, and personnel should be notified immediately. People with confirmed monkeypox infection who do not require hospitalization should be isolated at home and implement isolation and infection control measures in a home setting (see technical bulletin: Infection Control and Prevention for Patients in a Home Setting).
Infection Control and Prevention for Health Care Providers
Human-to-human transmission of monkeypox virus occurs by direct contact with lesion material or from exposure to respiratory secretions. Reports of human-to-human transmission describe close contact with an infectious person.
Transmission in health care settings has been rarely described.1 However, health care providers who might encounter patients with monkeypox or patients exposed to monkeypox should familiarize themselves with the necessary infection prevention and control measures. These measures were described in a previous DPBH technical bulletin, Infection Control and Prevention in Healthcare Settings.
Additional recommendations for infection prevention and control of monkeypox in health care settings provided by the CDC include:
Patient placement: A patient with suspected or confirmed monkeypox infection should be placed in a single-person room; special air handling is not required. The door should be kept closed (if safe to do so). The patient should have a dedicated bathroom. Transport and movement of the patient outside of the room should be limited to medically essential purposes. If the patient is transported outside of their room, they should use well-fitting source control (e.g., medical mask) and have any exposed skin lesions covered with a sheet or gown. Intubation, extubation and any procedures likely to spread oral secretions should be performed in an airborne infection isolation room.
Personal protective equipment (PPE): Health care personnel caring for patients with suspected or confirmed monkeypox should wear a gown, gloves, eye protection (e.g., goggles or face shield), and a NIOSH-approved particulate respirator with N95 filters or higher.
Environmental infection control:
- Standard cleaning and disinfection procedures should be performed using an EPA-registered hospital-grade disinfectant with an emerging viral pathogen claim (EPA’s List Q). Follow the manufacturer’s directions for concentration, contact time, and care and handling.
- Soiled laundry (e.g., bedding, towels, clothing) should be handled in accordance with recommended standard practices, avoiding contact with lesion material that may be present on the laundry.2 Soiled laundry should be gently and promptly contained in an appropriate laundry bag and never be shaken or handled in manner that may disperse infectious material.
- Appropriate PPE should be worn when entering a patient’s room and when handling contaminated or potentially contaminated materials.
- Activities that could resuspend dried materials from lesions such as dry dusting, sweeping, use of portable fans or vacuuming should be avoided. Wet cleaning methods are preferred.
- Management of food service items should also be performed in accordance with routine procedures.
Waste management: Handling, storage, treatment and disposal of soiled PPE, patient dressings, etc. should be performed in accordance with U.S. Department of Transportation (DOT) Hazardous Materials Regulations (HMR; 49 CFR parts 171-180.)3
Infection prevention precautions should continue until a decision has been made in consultation with the local health department to discontinue precautions.
Clinicians should contact their local public health authority (see reporting section, below) as soon as monkeypox is suspected.
Duration of isolation precautions for patients with suspected or confirmed monkeypox infection in a health care setting:
- Those with suspected monkeypox infection should have recommended isolation precautions for monkeypox maintained until monkeypox infection is ruled out.
- Those with confirmed monkeypox infection should have recommended isolation precautions for monkeypox maintained until all lesions have crusted, those crusts have separated, and a fresh layer of healthy skin has formed underneath.
Decisions regarding discontinuation of isolation precautions in a health care facility may need to be made in consultation with the local or state health department, depending on the jurisdiction.
Monitoring of Patients with a Monkeypox Virus Exposure
In general, patients in health care facilities who have had a monkeypox virus exposure and are asymptomatic do not need to be isolated, but they should be monitored. Monitoring should include assessing the patient for signs and symptoms of monkeypox, including a thorough skin exam at least daily for 21 days after their last exposure. They should receive post-exposure management according to current recommendations.
During the 21-day monitoring period:
- If a rash occurs, patient should be placed on empiric isolation precautions for monkeypox until (1) the rash is evaluated; (2) testing is performed, if indicated; and (3) the results of testing are available and are negative.
- If other symptoms of monkeypox infection are present, but there is no rash, patients should:
- Be placed on empiric isolation precautions for monkeypox for 5 days after the development of any new symptom, even if this 5-day period extends beyond the original 21-day monitoring period.
- If 5 days have passed without the development of any new symptom and a thorough skin and oral examination reveals no new rashes or lesions, isolation precautions for monkeypox can be discontinued.
- Isolation precautions may be discontinued prior to 5 days if monkeypox has been ruled out.
- If a new symptom develops again at any point during the 21-day monitoring period, then the patient should be placed on empiric isolation precautions for monkeypox again, and a new 5-day isolation period should begin.
- Be placed on empiric isolation precautions for monkeypox for 5 days after the development of any new symptom, even if this 5-day period extends beyond the original 21-day monitoring period.
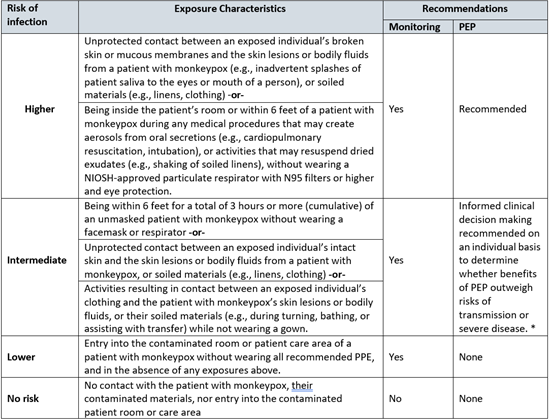
Assessing Risk of Health Care Provider with Monkeypox Virus Exposure
The table below is intended to highlight each risk level category by showing the need for monitoring and recommendations for postexposure prophylaxis (PEP).4 The exposure risk level of any incident may be recategorized to another risk level at the discretion of occupational health services or public health authorities due to the unique circumstances of each exposure incident. Health care providers (HCPs) who enter a contaminated patient room or care area while wearing recommended PPE should be aware of the signs and symptoms of monkeypox; if any signs or symptoms of monkeypox occur, HCP should notify occupational health services for further evaluation and should not report to work (or should leave work, if signs or symptoms develop while at work).
How to Monitor Health Care Provider Exposure
Decisions on how to monitor exposed HCP are at the discretion of the occupational health program and public health authorities. In general, the type of monitoring employed often reflects the risk for transmission with more active- monitoring approaches used for higher risk exposures. Self-monitoring approaches are usually sufficient for exposures that carry a lesser risk for transmission. Even higher risk exposures may be appropriate for a self-monitoring strategy if occupational health services or public health authorities determine that it is appropriate. Ultimately, the person’s exposure risk level, their reliability in reporting symptoms that might develop, the number of persons needing monitoring, time since exposure, receipt of PEP, and available resources, are all factors when determining the type of monitoring to be used. See when to use work restrictions to determine when HCP’s need to be excluded from work due to exposure or illness.
Reporting of Possible Cases
Patients that may have monkeypox or who might have been exposed to someone with monkeypox are required to be reported to public health authorities. Contact the appropriate health authority to report potential cases of monkeypox or for clinical consultation.
| Health Department | County | Phone Number to Report |
| Southern Nevada Health District (SNHD) | Clark | (702) 759-1300 (24 hours) |
| Washoe County Health District (WCHD) | Washoe | (775) 328-2447 (24 hours) |
| Carson City Health and Human Services (CCHHS) | Carson City, Douglas and Lyon counties | (775) 887-2190 (24 hours) |
| Nevada Division of Public and Behavioral Health (DPBH) | All other counties | (775) 684-5911 (M-F 8 am to 5 pm) (775) 400-0333 (after hours) |
Questions:
For updated guidance, review the DPBH Technical Bulletin web page. Email stateepi@health.nv.gov for other questions regarding monkeypox.

