RSV, Influenza and COVID-19
Background:
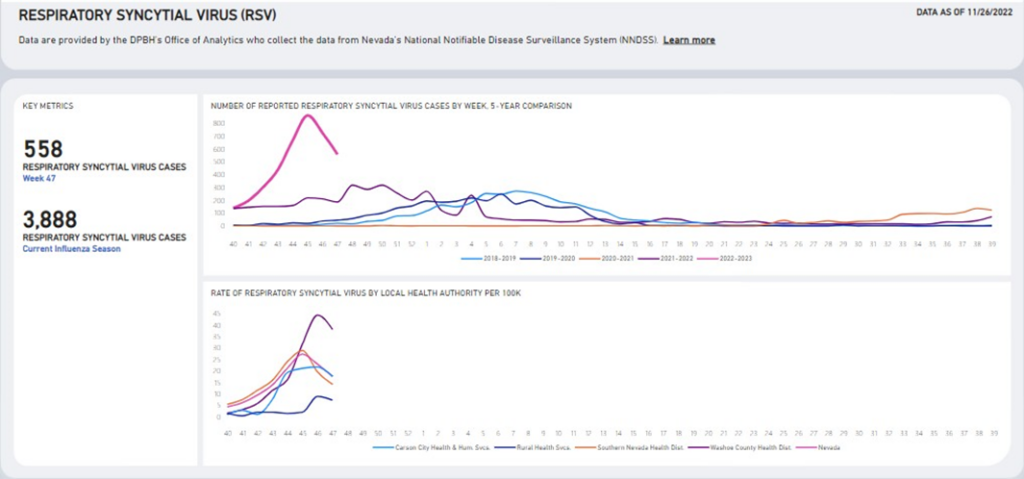
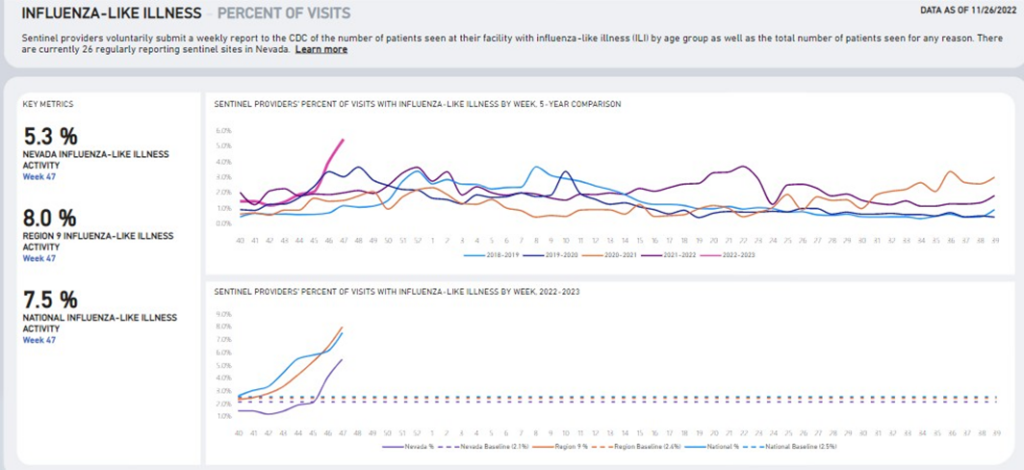
The season of respiratory viral infections typically begins in the fall and continues through the spring, with peak periods usually between December and February, but can vary each year. The Nevada Department of Health and Human Services (DHHS) Division of Public and Behavioral Health (DPBH), conducts routine surveillance for influenza, respiratory syncytial virus (RSV), and COVID-19. Current data indicates that these respiratory viruses are co- circulating within Nevada. In addition, influenza and RSV are spreading at higher rates than in recent seasons. This increase in transmission is resulting in healthcare capacity issues especially related to RSV within pediatric intensive care units, neonatal intensive care units and general pediatric units across Nevada hospitals. DHHS encourages providers to perform testing for these respiratory viruses to help inform treatment and ongoing prevention measures. Having conversations with patients regarding prevention measures, including promotion of vaccination, staying home when sick, hand hygiene, respiratory etiquette and mask wearing, is recommended to help decrease transmission rates. In addition to the COVID-19 dashboard, DHHS also provides weekly data for influenza and RSV, which can be found here (see sample screen shots below).
Symptoms and Transmission:
Many symptoms of influenza, RSV and COVID-19 are similar and may include:
- Fever or feeling feverish/having chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Sore throat
- Runny or stuffy nose
- Muscle pain or body aches
- Headache
- Vomiting and diarrhea
- Change in or loss of taste or smell, although this is more frequent with COVID-19.
All three respiratory viruses are spread from person-to-person among people who are in close contact with someone who is ill. Respiratory viruses are spread mainly by large and small particles that are expelled when people with the illness cough, sneeze or talk. These particles land in the mouths and noses of people who are in close proximity and may be inhaled into their lungs. Although most respiratory viruses are spread by inhalation, it may also be possible for people to become infected by touching a contaminated surface and then touching their own mouth, nose or eyes.1,2
Testing:
The only way to determine if a person is infected with influenza, RSV and/or COVID-19 is to perform testing. There are many testing options for these respiratory viruses, which include laboratory-based molecular tests and rapid point-of-care tests. There are also combination molecular tests available to test for COVID-19 and influenza simultaneously. It is possible for individuals to be infected with more than one respiratory virus at the same time. Testing options for these respiratory viruses include the following:
COVID-19
Influenza
RSV
Isolation/Exclusion Timelines:
Every infectious disease has its own unique infectious period, transmissibility and isolation period. Once laboratory identification has occurred to diagnose either COVID-19, influenza and/or RSV it is important for the infected person to remain isolated appropriately to protect others from being exposed to and contracting the respiratory viral infection.
- RSV: Any individual who tests positive for RSV must isolate at home until their fever is gone for at least 24 hours without the use of fever-reducing medications and they are well enough to participate in routine activities.
- Influenza: Any individual who tests positive for influenza must isolate at home until fever is gone for at least 24 hours without the use of fever-reducing medications and they are well enough to participate in routine activities.
- COVID-19:
- General public
- Any individual who tests positive for COVID-19, regardless of whether they are symptomatic and regardless of vaccination status, must isolate at home for 5 days.
- Day “0” for those with symptoms is the day that symptoms began. For those with asymptomatic infections, day “0” is the date of specimen collection for the positive test result.
- Persons may leave their house after 5 days if they have no symptoms or if their symptoms are resolving*.
- Persons should continue to wear a mask around others for 5 additional days.
- Some people with severe illness (e.g., requiring hospitalization, intensive care, or ventilation support) may produce replication-competent virus that may warrant extending the duration of isolation and precautions for up to 20 days after symptom onset.
- Any individual who tests positive for COVID-19, regardless of whether they are symptomatic and regardless of vaccination status, must isolate at home for 5 days.
- Health care personnel
- CDC recommends three different strategies for addressing health care personnel who test positive for COVID-19, regardless of whether they are symptomatic and regardless of their vaccination status:
- Conventional strategy
- Isolate for 10 days, or 7 days with a negative test if asymptomatic or symptoms are resolving*
- Contingency strategy**
- Isolate for 5 days with/without a negative test if asymptomatic or symptoms are resolving*
- Crisis strategy**
- No work restriction, with prioritization considerations (e.g., asymptomatic or symptoms are resolving*)
- Conventional strategy
- CDC recommends three different strategies for addressing health care personnel who test positive for COVID-19, regardless of whether they are symptomatic and regardless of their vaccination status:
- General public
* Symptoms resolving is defined as at least 24 hours fever-free without the use of fever-reducing medication and other symptoms are improving (loss of taste and smell might last for weeks or months after recovery but should not delay ending isolation)
** Facilities should consider implementing staffing shortage mitigation plans based on CDC recommendations described online here. Facilities with questions regarding implementing staffing shortage mitigation plans should contact the Office of Public Health Epidemiology and Investigations (OPHIE) at outbreak@health.nv.gov or the Nevada Bureau of Health Care Quality and Compliance (HCQC) Infection Prevention team at hcqcipcteam@health.nv.gov.
Vaccination:
Currently there is no vaccine to protect against RSV. However, both influenza and COVID-19 vaccinations are readily available and provide the best protection against these respiratory viruses and their potentially serious complications. Getting vaccinated combined with other mitigation measures not only protects those vaccinated and their close contacts, but also preserves our health care capacity by reducing the number of people who need medical attention related to complications.
- Influenza vaccination is available for those aged 6 months and older and is recommended to support personal health and protect the overall health of the public. CDC’s seasonal influenza vaccination resources for health professionals can be found online here.
- COVID-19 vaccines are available for those aged 6 months and older. Promotion of COVID-19 vaccine is crucial to controlling and eventually ending the current pandemic. It is also important to establish trust and confidence in the vaccine. More information regarding COVID-19 vaccine can be found online here.
Basic Prevention Measures:
Layering prevention strategies can help prevent severe illness and reduce the potential for strain on the health care system. In addition to isolation and vaccination, individuals should be encouraged to avoid others who are sick, cover coughs and sneezes, wear a mask and wash hands for at least 20 seconds with soap and water. 3
Questions:
For updated guidance, review the DPBH Technical Bulletin web page linked here and Nevada’s COVID-19 response website regularly. Email stateepi@health.nv.gov with questions.
References:
1 https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm
2 https://www.cdc.gov/rsv/about/transmission.html
3 https://www.cdc.gov/hygiene/personal-hygiene/coughing-sneezing.html

