Section IV
Guidelines: Environment and Sanitation
A. Cleaning, Sanitizing, and Disinfection
This section provides general information about cleaning, sanitizing, and disinfecting; guidelines for specific items commonly used in the childcare and school setting; and a checklist for choosing a disinfectant other than bleach.
- Definitions
Cleaning – Mechanical process (scrubbing) using soap or detergent and water to remove dirt, debris, and many germs. It also removes invisible debris that interferes with disinfection.
Sanitizing – Chemical process of reducing the number of disease-causing germs on cleaned surfaces to a safe level. This term is usually used in reference to food contact surfaces or mouthed toys or objects.
Disinfecting – Chemical process that uses specific products to destroy harmful germs (except bacterial spores) on environmental surfaces.
- General information
- Lessen the harmful effects of germs (bacteria, fungus, parasites, and viruses) by keeping their numbers low.
- Control germs effectively by frequent, thorough hand washing; cleaning and disinfecting frequently touched surfaces and objects that come in contact with children; and proper handling and disposal of contaminated items.
- Follow proper cleaning and disinfecting practices whether dirt is seen or not. Germs can live on wet and dry surfaces and on those items that do not look soiled or dirty.
- Increase the frequency of cleaning and disinfecting to control certain communicable diseases.
- Treat all body fluids as infectious because disease-causing germs can be present even in the absence of illness.
- Know that children who do not show symptoms of illness may be as infectious as those children who do have symptoms.
- Glove use
- Wear disposable gloves (consider using non-latex gloves as a first choice) when:
– Handling blood (e.g., nosebleeds, cuts) or items, surfaces, or clothing soiled by blood or body fluids.
– Covering open cuts, sores, or cracked skin.
– Cleaning bathrooms, diapering areas or any areas contaminated with stool, vomit, or urine.
- Remove gloves properly and discard after each use.
- ALWAYS WASH HANDS IMMEDIATELY when gloves are removed. Also wash hands when there has been contact with any body fluids. Follow hand washing and gloving procedures.
- When using cleaning, sanitizing, or disinfecting products ALWAYS:
- Consider the safety of children.
- Choose a product appropriate for the task.
- Follow the label instructions for mixing, using, and storing solutions.
- Read the warning labels.
- Store these products safely and out of reach of children.
- Clean soiled surfaces and items before using sanitizers or disinfectants.
- Cleaning
- Use warm/hot water with any household soap or detergent.
- Scrub vigorously to remove dirt and soil. Use a brush if item is not smooth or has hard to reach corners, such as toys and bottles.
- Change water when it looks or feels dirty, after cleaning bathrooms and diaper changing area, and after cleaning the kitchen.
- Always clean the least dirty items and surfaces first (for example, countertops before floors, sinks before toilets).
- Always clean high surfaces first, then low surfaces.
- Disposable towels are preferred for cleaning. If using reusable cloths/rags, launder between cleaning uses. DO NOT use sponges since they are hard to clean.
- Clean completely on a regular schedule and spot clean as needed.
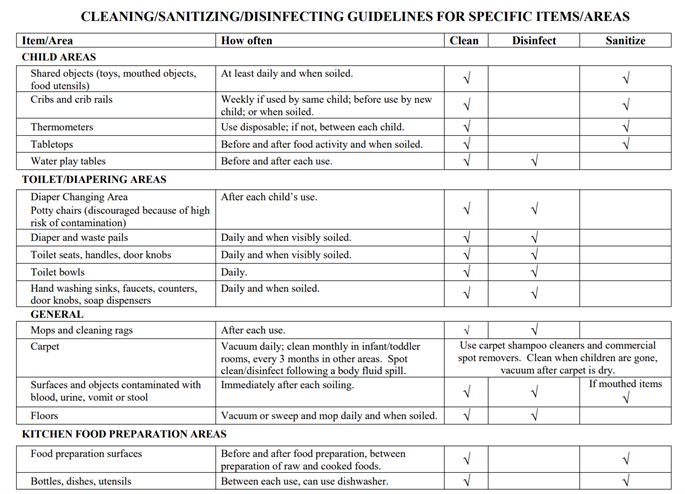
- Sanitizing or Disinfecting Products (See IV-8 for guidelines for specific items)
- Bleach (Sodium hypochlorite)
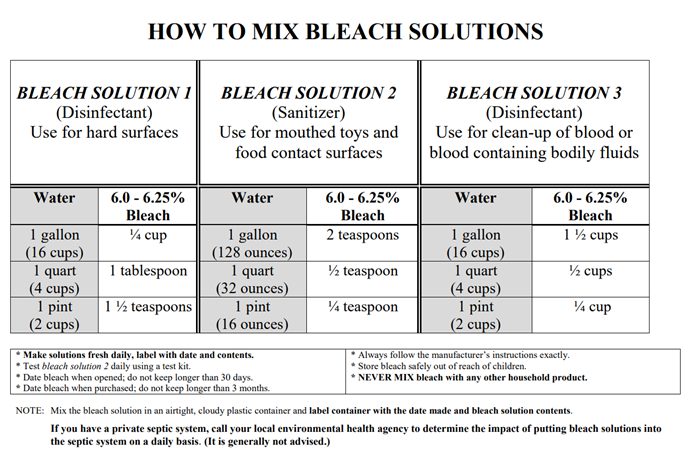
Bleach solutions of differing concentrations can be used for sanitizing and disinfecting. You can prepare your own bleach solutions by mixing specified amounts of household bleach and water (see IV-7 for how to mix different solutions and for information on handling, storage, and safety concerns), or you can purchase commercially prepared bleach-containing products. Make sure the bleach solution is appropriate for the type of item to be sanitized or disinfected.
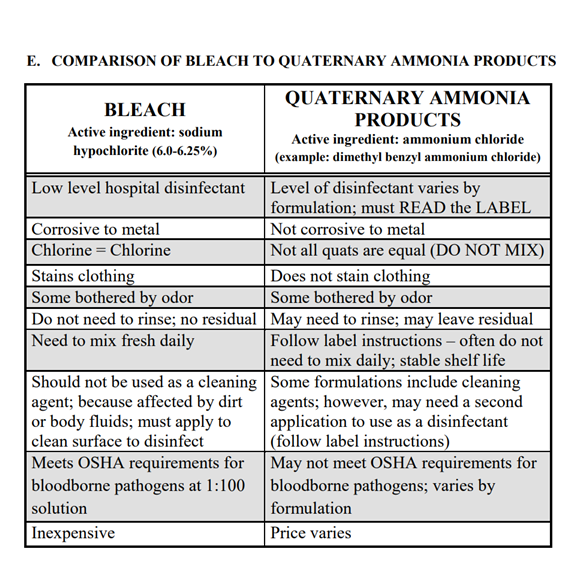
Bleach is safe when used as directed, is effective against germs when used at the proper concentration, is inexpensive if you make your own solutions, and is readily available. However, bleach is corrosive to metals and can strip floor wax, is ineffective in the presence of body fluids and soil (you must always clean first), is unstable when mixed with water (needs to be made fresh daily) and can be dangerous if mixed with other products.
– Bleach solution 1 – disinfectant (See IV-7)
This solution contains approximately 800 parts per million (ppm) of sodium hypochlorite. Use to disinfect surfaces that will not have contact with food or the mouth (e.g., changing tables, potty chairs, activity tables, floors).
This solution is recommended by the Centers for Disease Control and Prevention, American Academy of Pediatrics, and American Public Health Association for use in childcares and schools where there is a high potential for fecal contamination. Your local environmental health professionals or licensing agency may have different recommendations.
– Bleach solution 2 – sanitizer (See IV-7)
This solution contains approximately 200 parts per million (ppm) of sodium hypochlorite. Use to disinfect mouthed toys and other objects, eating utensils, and food-contact surfaces.
While a bleach solution of 200 ppm is recommended for mouthed toys, it’s important to note the FDA Food Code states that the range of the sanitizing solution must be from 50- 100 ppm. It must not exceed 100 ppm. Chlorine test kits are available for purchase to check the concentration of your solution. Commercially licensed facilities are required to use a test kit to measure the strength of the sanitizing solution.
- Quaternary ammonia products (QUATS)
There are many types of quaternary ammonia products, and they are not all the same. However, a common chemical name of the active ingredient is dimethyl benzyl ammonium chloride. It is important to read the label and to follow the instructions carefully to make sure you are using a product that is appropriate for the type of item to be sanitized or disinfected.
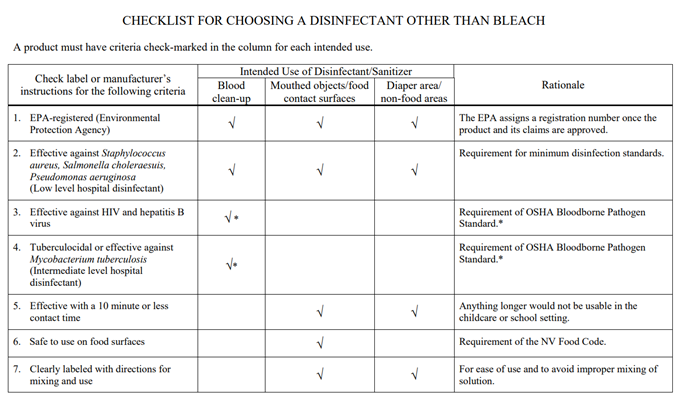
Use the checklist to determine if the product meets the criteria for both a sanitizer and/or disinfectant. For example, if using for disinfection after a blood spill or splatter, it must meet OSHA requirements for the blood borne pathogen exposure plan, that is, be EPA-registered as tuberculocidal, or list that HIV and hepatitis B viruses are killed by the product.
Use test kit daily to monitor the correct concentration of the product used in the food areas (200-400 ppm). A separate test kit is needed to measure the concentration of the QUAT solution. Obtain test kits from your chemical supplier. Use separate bottles and label each clearly with its intended use with the name of product, date mixed, food/mouth-contact use, or general disinfection. Always STORE OUT OF CHILDREN’S REACH – undiluted QUATS can be fatal if ingested.
REMEMBER when using QUATS:
Read the label and follow the manufacturer’s directions exactly for the following procedures:
– how to mix product.
– how to apply the solution.
– how long to leave on the surface.
– whether to rinse after exposure time.
– safety concerns when used around children.
The solution for use on food contact surfaces may differ from that used for general disinfection. Read the label and follow the directions exactly. For more information about a specific product call the distributor or the company. The 1-(800) number is usually found on the product label.
- Other sanitizing or disinfecting products
Use the checklist in the following section or go to EPA Pesticide Product Label System to determine if a product can be used in your facility. Always read the label and follow the directions carefully.
- Disinfecting Procedures
- Surfaces or objects that will NOT have contact with the mouth or food (immediately after each soiling) e.g., chairs, desks, etc.
-
- Clean first with soap or detergent and water.
- Rinse.
- Spray the area thoroughly with Bleach Solution 1 (See IV-7) or another appropriate disinfecting product.
- Wipe the area to distribute the disinfectant evenly using single-service, disposable paper towels.
- Discard paper towels in a plastic-lined container.
- Allow surface to air dry.
- Wash your hands.
- Water play tables (before and after each use)
-
- Wipe table with bleach solution 1 or another appropriate disinfecting product.
- Let dry before filling with water.
- Soak all water table toys in bleach solution 2 or another appropriate sanitizing product for two minutes prior to use.
- Ensure that all children and staff wash hands before and after play.
- Exclude any child with open sores or wounds from play.
- Watch carefully so children do not drink the water.
- Drain the water after play is over and between groups of children.
- Clean with soap or detergent and water.
- Blood and body fluid spills or soiling
-
- Wear disposable medical gloves for any blood and body fluid cleanup.
- Use disposable towels to ALWAYS clean objects and surfaces contaminated with blood and body fluids (stool, urine, vomit) and discard in a plastic-lined, covered waste container.
- Scrub the area with soap or detergent and water to remove blood or body fluids and discard paper towels. Rinse the area with clean water.
- Disinfect immediately using bleach solution 1 or another appropriate disinfecting product on any items and surfaces contaminated with blood and body fluids (stool, urine, vomit).
- Allow surface to air dry.
- Discard disposable gloves. If using utility gloves, follow cleaning/disinfecting procedure.
- Wash hands immediately.
- Washable items like linens, towels, bedding
-
- Use hot water in a washing machine. This is acceptable for soaking, cleaning, sanitizing, and disinfecting washable articles.
- Read the label on the laundry detergent.
- Read the label and follow directions exactly if using bleach.
- Dry items in a dryer on high heat.
- Sanitizing Procedures
- Surfaces that come in contact with food or are mouthed
-
- Clean first with soap or detergent and water.
- Rinse.
- Spray the area thoroughly with bleach solution 2 or another appropriate sanitizing product.
- Wipe the area to evenly distribute the sanitizer using single-service, disposable paper towels.
- Discard paper towels in a plastic-lined container.
- Allow to air dry.
- Items in contact with food or are mouthed (toys, eating utensils, dishes, formula bottles)
– Three separate sinks (or basins) method
-
- Sink/Basin #1: wash items in hot water using detergent (bottle brushes as needed).
- Sink/Basin #2: rinse in clear water.
- Sink/Basin #3: soak items in bleach solution 2 for at least two minutes.
- Remove items, DO NOT rinse, and place on rack to air dry.
– Dishwashers
To be acceptable a dual process for cleaning with the detergent and agitation and sanitizing with heat or chemicals must be provided.
Two types are available, commercial, and household:
♦ National Sanitation Foundation (NSF) approved commercial dishwashers are required in commercial childcare or school food service. The NSF standards require that the water temperature reach 180° F, or that there is 50 ppm chlorine in the final rinse of the dishwasher.
♦ Household dishwashers must have a heat sanitizing setting. If at the end of the cycle when the machine is opened the dishes are too hot to touch, then the items are sanitized. It is strongly recommended that household dishwashers carry the NSF mark of approval.
- Green Cleaning Products
There has been an increased interest in using “green” cleaning products in childcare settings, schools, and homes. This interest is twofold: first is due to reports about increased allergies, sensitivities and illness in children associated with chemical toxins in the environment and second, these products tend to cause less damage to the environment.
Children are more vulnerable to chemical toxins because of their immature immune systems, rapidly developing bodies, and their natural behaviors. They play on the floor, are very tactile having much body contact with the tables, desks, or play equipment, and have oral behaviors of mouthing toys and surfaces and putting their hands in their mouths frequently.
Green cleaning products can be used in childcare and school settings. Green sanitizers or disinfectants must meet the criteria on page IV-9 and be approved by your local environmental health agency or your childcare consultant.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
B. How to Mix Bleach Solutions
Adapted from the Hennepin County, Minnesota Human Services and Public Health Department’s Infectious Diseases in Childcare Settings and Schools Manual and/or the Washoe County Nevada Health Department’s Infectious Diseases in Childcare Settings and Schools Manual.
C. Cleaning/Sanitizing/Disinfecting Guidelines for Specific Items/Areas (Poster)
Adapted from the Hennepin County, Minnesota Human Services and Public Health Department’s Infectious Diseases in Childcare Settings and Schools Manual and/or the Washoe County Nevada Health Department’s Infectious Diseases in Childcare Settings and Schools Manual.
D. Checklist For Choosing a Disinfectant Other than Bleach
Adapted from the Hennepin County, Minnesota Human Services and Public Health Department’s Infectious Diseases in Childcare Settings and Schools Manual and/or the Washoe County Nevada Health Department’s Infectious Diseases in Childcare Settings and Schools Manual.
E. Comparison of Bleach to Quaternary Ammonia Products
Adapted from the Hennepin County, Minnesota Human Services and Public Health Department’s Infectious Diseases in Childcare Settings and Schools Manual and/or the Washoe County Nevada Health Department’s Infectious Diseases in Childcare Settings and Schools Manual.
F. Diapering
- General information
Childcare providers and school health staff can help prevent the spread of infectious organisms by changing diapers in a separate designated area and by using effective cleaning and disinfecting practices. Germs found in the stool can be spread when the hands of caregivers or children contaminate objects, surfaces, or food. Infections that can be spread by contact with stool include bacteria (e.g., Salmonella, Shigella, Campylobacter), parasites (e.g., Cryptosporidium, Giardia, pinworms), and viruses (e.g., rotavirus, norovirus, hepatitis A virus).
Note: The importance of using good body mechanics cannot be over emphasized when changing diapers of larger or older children, as well as infants and toddlers. Use appropriate bending and lifting techniques to prevent injury.
- Basic principles
- Change diapers in a designated diapering area.
- Follow safety procedures and do not leave children unattended.
- Use surfaces that can be easily cleaned and disinfected.
- Use a separate area for diapering that is away from the medication, food storage, food preparation, and eating areas.
- Dispose of soiled diapers in a covered waste container.
- Wash hands of both staff and children after diapering.
- DO NOT allow objects such as toys, blankets, pacifiers, or food in the diapering areas.
- Consult with your childcare health consultant or school nurse for any special diapering issues.
- Equipment
- Changing surface
– The changing surface should be separate from other activities.
– The surface should be smooth, moisture-resistant, and of an easily cleanable material.
– For extra protection use a non-absorbent, disposable paper under the child. – The changing surface should be next to a hand washing sink.
- Hand washing sink and supplies
– Adequate hand washing facilities should be available to school staff when diapering children in school settings.
– The hand washing sink should be equipped with both hot and cold running water mixed through one faucet (hot water temperature not greater than 1200 F).
– The water controls should ideally be foot-operated or knee-operated to avoid contamination of hands and/or water controls. If faucets are not foot-operated or knee-operated, turn off faucet handles with a disposable paper towel.
– The changing sink should not be the same as the food preparation sink.
– Liquid soap, paper towels, and fingernail brush should be within reach.
– Single-service, disposable towels should be used instead of cloth towels.
- Hand washing procedures
The hands of the provider and child must be washed after each diaper change. Refer to hand washing information on pages II-4 through II-7. Check with your childcare health consultant or school nurse to determine which hand washing procedures are appropriate for different age groups of children.
- Diapers
- High-absorbency disposable diapers are preferred because cloth diapers do not keep stool and urine contained as well as disposable diapers and require more handling (the more handling, the greater opportunity to spread germs).
- All diapers must have an absorbent inner lining completely contained within an outer covering made of waterproof material that prevents the escape of stool and urine.
- Soiled clothing should be placed in a plastic bag and sent home each day.
- Cloth diaper considerations
- The outer covering and inner lining must both be changed with each diaper change.
- Outer coverings must not be reused until they are laundered.
- Each child should have an individually labeled, covered, and plastic-lined diaper pail.
- Soiled diapers or clothing should NOT be rinsed in sinks or toilets.
- The diaper or clothing soiled with stool must be put in separate plastic bags before placing into the diaper pail.
- Soiled cloth diapers and/or clothing should be sent home each day in clean plastic bags.
- An adequate supply of diapers and diaper coverings must be available for each day.
Diapering procedures, see IV-15. Changing pull-ups/toilet learning procedures, see IV-16.
- Disposable gloves
- Non-latex gloves without powder should be considered because of possible allergy to latex in staff and children.
- Gloves should be worn when changing the diaper of a child with diarrhea or a known infection that is spread through the stool.
- Pregnant women or women considering pregnancy should wear gloves when changing any diaper.
- Staff should wear gloves if they have open cuts, sores, or cracked skin, or if the children have open areas on their skin.
- Gloves should be discarded, and hands washed after each diaper change.
- Gloves must be single use only. Food service gloves are not appropriate.
- Disposable wipes
- A sufficient number of pre-moistened wipes should be dispensed before starting the diapering procedure to prevent contamination of the wipes and/or the container.
- Each child should have an individually labeled container of wipes that is not shared with others. Put the child’s full first and last name on the container.
- Skin care items
- Childcare providers and schools must have policies regarding use of these products. Parents/guardians or healthcare providers must provide written, signed directions for their use.
- If skin care items are used, keep them within the provider’s reach and out of the reach of children.
- Each child must have an individually labeled container of skin care products that is not shared with others. Label the container with the child’s full first and last name.
- Skin care products must be used according to package directions.
- Plastic bags
- Disposable plastic bags must be used to line waste containers and to send soiled clothing or cloth diapers home.
- Plastic bags must be stored out of children’s reach.
- Waste containers and diaper pails
- A tightly covered container, preferably with a foot-operated lid, is recommended.
- The container must be kept away from children.
- The container must be lined with a disposable plastic trash bag.
- The waste container should be emptied before full and at least daily.
- The container should be cleaned with detergent and water, rinsed, and disinfected daily.
- Potty chair or commodes (not recommended)
- Flush toilets are recommended rather than commodes or potty chairs. However, if potty chairs or commodes are used, frames should be smooth and easy to clean.
- Empty the potty chair or commode into the toilet, clean with soap and water, rinse, and disinfect after each use. Empty dirty cleaning water into the toilet and not the hand sink.
- If a potty chair or commode has wheels, lock wheels into position while using.
- Utilize proper body mechanics when moving and positioning a child on a potty chair or commode.
- Cleaning and disinfecting supplies needed
- Disposable gloves and towels.
- Cleaning solution.
- Disinfecting solution (Bleach solution 1 or another appropriate disinfecting product).
- Disinfecting procedures
-
- Clean first with soap or detergent and water.
- Rinse.
- Spray the area thoroughly with Bleach solution 1 or another appropriate disinfecting product.
- Wipe the area to distribute the disinfectant evenly using single-service, disposable paper towels.
- Discard paper towels in a plastic-lined container.
- Allow surface to air dry.
- Wash your hands.
If you have questions about cleaning and disinfecting procedures, ask your childcare health consultant or school nurse for specific instructions.
G. Food Safety in Childcare Settings and Schools
Foodborne illness can be prevented by following guidelines for: hand washing, excluding ill foodservice workers, and for storing, handling, preparing, and cooking food and beverages in the childcare and school settings.
- Hand washing
Wash hands thoroughly with soap and warm running water after using the toilet, changing diapers, and before preparing or eating food. Thorough hand washing is the best way to prevent the spread of communicable diseases. Alcohol-based hand rubs are not acceptable in the food service area. (See Hand Washing section of this manual for more information on hand washing.)
- Exclusion
- People should not prepare or serve food with the following:
- vomiting and/or diarrhea or until 48 hours after the last episode of vomiting or diarrhea.
- until treated with antibiotics or have had one or more negative stool tests (depends on specific bacteria).
- skin lesions on exposed areas (face, hands, fingers) that cannot be covered. Wear finger cots or disposable gloves over covered sores on the fingers or hands.
- when wearing fingernail polish.
- See also: NRS 446.935
- Food and beverage storage, handling, preparation, and cooking guidelines
- Storage guidelines/rationale
The following foods may not be served or offered for sale in a ready-to-eat form:
(a) Raw animal foods, including, without limitation, raw fish, raw marinated fish, raw molluscan shellfish and steak tartare;
(b) A partially cooked animal food, including, without limitation, lightly cooked fish, rare meat, soft-cooked eggs made from raw eggs and meringue; and
(c) Raw seed sprouts.
– Store all potentially hazardous foods (eggs, milk or milk products, meat, poultry, fish, etc.) at 41° F or below. Childcare centers/schools that receive hot food entrees must hold potentially hazardous foods at 140° F and above and check food temperature with a clean, calibrated food thermometer before serving. Bacteria may grow or produce toxins if food is kept at temperatures that are not hot or cold enough. These bacteria can cause illness if the food is eaten. Store lunches that contain potentially hazardous foods in the refrigerator. Use coolers with ice packs for keeping lunches cold on field trips.
– Store raw meat and poultry products on the bottom shelf of the refrigerator. This will help to prevent the meat and poultry juices from dripping onto other foods.
– Keep food products away from cleaning products, medicine, and animal food. Never refer to medicine as “candy” as this may encourage children to eat more medicine than they should. Some cleaning products can be mistaken for foods. For example, cleansers may look like powdered sugar and pine cleaners may look like apple juice. Cleaning products must be properly labeled.
- Preparation guidelines/rationale
– Prepare food in an approved preparation area. Preferably, one sink should be dedicated for food preparation and one for hand washing. This area has equipment, surfaces, and utensils that are durable, easily cleaned, and safe for food preparation.
– Rinse fresh produce in a clean, sanitized sink before preparing. This helps remove pesticides or trace amounts of soil and stool, which might contain germs that may be on the produce.
– Clean all surfaces before beginning food preparation. Unclean surfaces can harbor bacteria and contribute to cross contamination. Cross contamination occurs when a contaminated product or its juices contacts other products and contaminates them.
– Use an approved sanitizer for food contact surfaces. Test kits can be used to check the concentration. High concentration of sanitizer can leave high residues on the food contact surface, which can contaminate food, make people ill, and damage surfaces or equipment. Follow the labeled instructions, especially if it calls for a rinse step after sanitizing.
– Label all sanitizer spray bottles. Check sanitizer solution daily using a test kit. Make a fresh solution if the concentration is below acceptable levels. This will prevent accidental misuse of sanitizer spray bottles.
– Always wash hands, cutting boards, utensils, and dishes between different foods. Use separate cutting boards for raw meats and produce. Cross contamination occurs when a contaminated product or its juices, (e.g., raw meat or poultry) touches other products (e.g., fresh fruit, vegetable, cooked foods) and contaminates them.
– Thaw foods properly:
1) on a tray on the bottom shelf of the refrigerator,
2) under continuously running cold (70° F or less) water in continuously draining sink, or
3) in the microwave, only if the food is cooked immediately afterwards. DO NOT leave food out on the kitchen counter to thaw. Thawing food on a kitchen counter can allow bacteria to grow in the food.
– DO NOT prepare infant formula in the hand washing sink area in the infant room. Use water from kitchen prep sink to mix infant formula or use bottled water.
- Cooking guidelines/rationale
– Use a trained, certified food handler to prepare food. Staff knowledgeable about safe food handling practices can prevent foodborne illnesses. Health departments may require certifications for commercial facilities.
– Rapidly heat potentially hazardous food. Take food temperatures to make sure food has reached appropriate temperature. Check with your local environmental health agency for appropriate temperatures. Rapid cooking kills bacteria that may cause illness.
– Cook raw hamburger thoroughly until juices run clear. Use a food thermometer to achieve an internal temperature of 155° F per NV Food Code. Raw or partially cooked ground beef can be contaminated with E. coli O157:H7. Large quantities of hamburger may “look” cooked but may contain “pockets” of partially cooked meat.
– Once cooked, take food temperatures to make sure food has reached appropriate temperature. Check with your local environmental health agency for appropriate temperatures. Monitoring temperatures can ensure that all potentially hazardous foods have not been in the “danger zone” (41° – 140° F) too long, which allows for bacterial growth.
– DO NOT put cooked food in the same container or on the same unwashed container, platter, or cutting board that was used for uncooked meat or poultry. The container or platter could contain harmful bacteria that could contaminate the cooked food.
– DO NOT serve unpasteurized milk, cheese, or apple juice. These items may be the source of foodborne illnesses caused by pathogens such as Campylobacter, Salmonella, E. coli O157:H7, and Listeria.
- Other Considerations
- DO NOT let children serve or prepare food in the childcare setting. Cooking projects in the childcare and school settings should be treated as a science project. Alternatively, have the children make an individual-sized portion for themselves.
- Children could contaminate food and make other children/staff ill if they handle food during these types of projects. Monitor the children’s hand washing and supervise children so they do not eat the food.
- If children bring food or treats to share, the food or treats must be purchased from a licensed store or bakery. DO NOT allow food/treats to be brought from home.
- Children and parents may not understand food safety principles as well as staff at licensed food establishments. Licensed commercial kitchens are more controlled environments for preparation than private homes.
- DO NOT wash bottles, nipples, or dishes in the hand washing sink area in the infant room.
- Any items that need to be cleaned and/or sanitized must be sent to the kitchen.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
H. Pets in Childcare Settings and Schools
The benefits of pet ownership outweigh the risks, but precautions are encouraged. If you choose to have an animal in the childcare or school setting, follow the listed guidelines to decrease the risk of spreading disease.
Check with your local health department or childcare licensing agency before bringing any pets to your childcare setting or school because there may be state and/or local regulations that must be followed.
For more information, see NAC 444.56834 (Nevada Sanitation Regulations) and NAC 432A.265 (Regulations for services and facilities for care of children).
- General considerations
- Inform parents/guardians of the benefits and potential risks associated with animals in the classroom.
- Consult with parents/guardians to determine special considerations needed for children with weakened immune systems and who have allergies or asthma.
- Notify parents/guardians of any child whose skin is broken by an animal bite or scratch.
- Supervise children when handling animals.
- Types of pets allowed in childcare and school settings include:
- guinea pigs
- gerbils
- domestic-bred rats
- rabbits
- dogs
- birds (must be free of Chlamydophila psittaci)
- fish
- domestic-bred mice
- hamsters
- cats
- Animals not recommended (and possibly not allowed) in school settings include:
– ferrets
– reptiles (e.g., lizards, turtles, snakes, iguanas)
– poultry (especially baby chicks and ducklings)
– inherently dangerous animals (e.g., lions, tigers, cougars, and bears)
– nonhuman primates (e.g., monkeys and apes)
– mammals at higher risk of transmitting rabies (e.g., bats, raccoons, skunks, and foxes)
– aggressive or unpredictable animals, wild or domestic
– stray animals with unknown health and vaccination history
– venomous or toxin-producing spiders, insects, reptiles, and amphibians
These animals are not allowed or recommended because:
– Reptiles and poultry can carry Salmonella bacteria and can be a source of infection to infants, children, and staff.
– Wild animals can be a source of infectious bacteria, parasites, viruses, and fungi.
– Biting incidents from animals are a concern especially from wild animals.
– In some municipalities, ordinances restrict wild/exotic animals and/or farm animals
- Where to keep pets
- Keep pets in designated areas only. They should be separated from food preparation, food storage, or eating areas.
- Keep pets in clean living quarters. Cages should be covered, sturdy, and easy to clean, and they should sit on surfaces that are solid and easy to clean.
- Care and maintenance
- Develop and follow written procedures concerning the care and maintenance of pets with the advice of your veterinarian.
- Assure that pets are appropriately vaccinated, free of parasites (this includes ticks, fleas, and intestinal worms), and fungal skin infections (e.g., ringworm).
- Keep animals that are in good health and show no evidence of disease. Healthy animals make better pets.
– Feed pets appropriate commercial foods on a regular basis and keep fresh water available at all times.
– Keep bedding dry and clean.
– Clean cages daily. School or childcare staff should do this – NOT children.
– Use a janitorial area to wash and clean cages or aquariums. DO NOT use the kitchen or food service sinks.
– Wash hands thoroughly after contact with animals and their cages.
- Minimize contact with urine and stool. Urine and stool not confined to an enclosed cage should be cleaned up immediately. Dispose of this waste in a covered container not accessible to children.
- WASH HANDS IMMEDIATELY after handling animals and their stool/urine and their environments.
- Check with local authorities (police) for regulations in your jurisdiction for appropriate disposal of a pet when it dies.
- Avoid changing cat litter boxes, handling animals, and contacting their environments if you are pregnant.
- Cover children’s sandboxes when not in use.
- Other considerations to reduce disease risks to children at petting zoos and farms
Germs can occur naturally in the gut of certain animals without causing the animal any harm. These germs are then shed into the environment in the stool of these animals. When people have contact with animals or their living areas, their hands can become contaminated. Disease spread can occur when dirty (unwashed, contaminated) hands go into the mouth or are used to cook or eat food.
- DO NOT allow children under 5 years to have contact with farm animals. These children are at greater risk for developing severe illness because their immune systems may not yet be fully developed.
- Educate childcare and school staff about the potential for transmission of enteric (intestinal) pathogens from farm animals to humans and strategies to prevent spread. Outbreaks of E. coli O157:H7, salmonellosis, and cryptosporidiosis have been attributed to children visiting farms and petting zoos.
Certain farm animals, including calves, young poultry, and ill animals, pose a greater risk for spreading enteric infections to humans.
- Apply childcare or school policies and procedures to animals brought in for show and tell, entertainment, or educational programs.
For information on Zoonotic Diseases in Nevada please visit www.onehealthnevada.com
- Prevention and control
- Wash hands to stop the spread of disease. Immediately after contact with animals, children and adults should wash their hands. Running water, soap, and disposable towels should be available. Adults should closely monitor hand washing of all children.
Wash hands after touching animals or their environments, on leaving the area in which the animals are kept, and before preparing or eating food. Emphasize these recommendations with staff training and posted signs. Communal wash basins are not adequate hand washing facilities. Where running water is not available, waterless hand sanitizers provide some protection.
- Assure that at farms or petting zoos:
– Two separate areas exist, one in which contact with the animals occurs and one in which animals are not allowed.
– Food and beverages should be prepared, served, and consumed only in animal-free areas.
– Toys and pacifiers should not be allowed in the animal contact areas.
– Animal contact should occur only under close adult supervision.
- DO NOT consume unpasteurized milk, apple cider, or juices.
- DO NOT eat unwashed fruits and vegetables.
- Consider the type of animals and the facilities before visiting an educational farm or petting zoo.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
I. Wading Pools
Wading pools have been identified as potential sources of disease transmission and as safety hazards. Nevada childcare licensing rules, for both centers* and family childcare homes, require that outdoor play areas be free of water hazards and potential sources of fecal contamination that could lead to transmission of enteric pathogens such as Cryptosporidium or Escherichia coli (E. coli) O157:H7.
* NAC 432A.250 subsection 4(h) states that play areas should not allow children access to any bodies of water.
According to reports from the Centers for Disease Control (CDC), each year, thousands of cases of E. coli O157:H7 infections are identified in the U.S. These often cause disruption of parents’ schedules and loss of income for the childcare provider because infected children need to be excluded from childcare until they are no longer carrying the bacteria, which can take as long as 1- 2 months. Several other disease-causing agents, including Giardia, Cryptosporidium, and Shigella are also efficiently transmitted in wading pools. All of these agents can cause severe illness in children.
Statistics on reported infectious diseases in Washoe County are available on the Northern Nevada Public Health ’s website; see Annual Communicable Disease Summary Reports.
Unlike swimming pools that are treated to prevent disease transmission, wading pools are typically filled with tap water and may or may not be emptied and disinfected on a daily basis. Thus, many enteric pathogens (germs from the stool) can be easily spread by contaminated wading pool water that children may accidentally swallow while playing in the pool.
Spread of these infections can occur even under the care of the most diligent and thoughtful childcare providers, since these infections can be spread even when the child only has mild symptoms. For these reasons, wading pools are not appropriate for childcare settings with infants and toddlers who are still in diapers.
In addition, children who are ill with vomiting or diarrhea due to enteric pathogens such as Cryptosporidium or E. coli O157:H7 should be kept out of pools for a specified time period even after the diarrhea has stopped. The Health District Epidemiology Dept. will work with the case and the facility to notify you when it is o.k. to participate in swimming or wading activities again.
In addition, the U.S. Consumer Product Safety Commission warns that young children can drown in small amounts of water, as little as two inches deep. Submersion incidents involving children usually happen in familiar surroundings and can happen quickly (even in the time it takes to answer the phone).
In a comprehensive study of drowning and submersion incidents involving children under 5 years old, 77% of the victims had been missing from sight for 5 minutes or less. The Commission notes that toddlers, in particular, often do something unexpected because their capabilities change daily. Child drowning is a silent death, since there is no splashing to alert anyone that the child is in trouble.
As an alternative to wading pools, sprinklers provide water play opportunities that are not potential hazards for drowning or disease transmission.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov
J. Clean-up of Public Vomiting Incidents’ (VPI’s), Feces, Blood and Other Body Fluids
Infectious diseases (e.g., viruses, bacteria, parasites, fungus) can be spread from person-to-person through contact with an infected person’s body fluids when they leave their body through coughing, sneezing, blood, vomit, stool and other body fluids.
Standardized cleanup of body fluids and excrement is a vital part of controlling the spread of disease. This means every clean up should be treated as though they are contaminated and capable of spreading disease and handled as such, no matter what the perceived reason is for the vomit, body fluid or fecal accident.
A public vomiting incident can be especially contagious as it not only contaminates the primary surface it lands on but also creates droplets that contaminate items and surfaces, they settle on. Performing a standardized PVI cleaning (25-foot radius surrounding the vomit incident and up to 6’ of any affected walls) will ensure any germs associated with the vomit will not infect others.
Clean-up Procedure
Cleaning is the mechanical process of scrubbing to remove dirt, debris, and large numbers of germs. Biofilms left on a surface can block the effects of a sanitizer or disinfectant and contribute to bacterial growth. It is important to remove the “visible” soil before sanitizing/disinfecting.
-
- Block off the area of the spill from persons walking by until cleaning and disinfecting are complete.
- Put on disposable gloves to prevent contamination of hands.
- Wipe up the spill using paper towels or absorbent material and place in a plastic garbage bag.
- Clean soiled areas with soap or detergent and hot water prior to sanitizing or disinfecting.
Gloves
Wear gloves when there is potential contact with vomit, body fluid or fecal material or contaminated items or surfaces.
- Wear gloves that fit appropriately (select gloves according to hand size)
- Do not wear the same pair of gloves for the cleanup of more than one incident
- Do not wash gloves for the purpose of reuse
- Thoroughly wash hands before putting gloves on and immediately after removing gloves Removal of gloves:
- Grasp edge of glove with opposite gloved hand; peel off from wrist to fingers inside out
- Hold removed glove in glove hand
- Slide ungloved fingers under the remaining glove at the wrist; peel off and discard
Sanitizing/Disinfecting Using Chemicals
Sanitizing/Disinfecting is the process in which a chemical or heat is used to reduce germs to a “safe” level for people to be around (the term sanitize is usually used in reference to cleaning food contact surfaces or mouthed toys or objects).
Recipe for 1,000 ppm Bleach Disinfecting Solution
- 9 parts cool water (1 gallon)
- 1 part household bleach (½ cup)
Add the household bleach to the water and gently mix the solution.
Bleach: One of the most commonly used and effective chemicals for disinfection is a homemade solution of household bleach and water. Since a solution of bleach and water loses its strength quickly, it should be mixed fresh at least every 24 hours.
Follow steps 1-4 in the cleaning procedure above then:
-
- Gently pour over or spray onto all contaminated areas and surfaces (25 ft. radius and 6ft high) using freshly made bleach solution or another FDA or EPA approved cleaner effective against hard to kill germs (e.g., norovirus, cryptosporidium, etc.)
- Follow manufacturer’s directions for contact time and any required water rinse wipe down (food surfaces or mouthed items).
- Wipe up the remaining solution.
- All non-disposable cleaning materials used such as mops and scrub brushes should be disinfected by saturating with a disinfecting solution and air dried.
- Remove gloves and place in plastic garbage bag with all soiled cleaning materials.
- Double-bag and securely tie-up plastic garbage bags and discard.
- Thoroughly wash hands with soap and water.
Sanitizing/Disinfecting Using Heat
Follow steps 1-4 in the cleaning procedure above then:
-
- Follow manufacturer’s directions for filling and use of the machine.
- To disinfect carpet & upholstery steam-clean with a minimum temperature of 170° F.
- Allow the carpet or upholstery to air-dry or dry with a fan (unit sits over the spot-does not blow across) before use and traffic resumes. Do not use dry or wet vacuum. Disinfect carpets and upholstery as soon as possible after the incident. Note: Wet carpets attract a great deal of dirt, so if it’s not possible to avoid walking on the carpet until it’s dry, lay some heavy-duty towels down, especially in high traffic areas. Be sure to remove the towels when the room is not in use so the carpet or upholstery will dry more quickly.
Things to remember and share with others
Although the environment cannot be made germ-free, keeping the number of germs in our environment at low levels can lessen their harmful effects. Frequent and thorough handwashing, cleaning and proper sanitizing or disinfecting of objects that come into contact with people, and proper handling and disposal of contaminated items, can most effectively control the number of germs we come into contact with.
- Clean completely on a regular schedule and spot clean as needed.
- Mix and store chemicals safely according to the label.
- Use 3 step process: clean, sanitize/disinfect, rinse.
For more information, please contact your local health department.
Southern Nevada Health District (Clark County) 702-759-1300 (24 hours)
Northern Nevada Public Health (Washoe County) 775-328-2447 (24 hours)
Carson City Health & Human Services (Carson City, Douglas, Lyon Counties) 775-887-2190 (24 hours)
Division of Public and Behavioral Health (All other Counties) 775-400-0333 (24 hours)
Email: dpbhepi@health.nv.gov

